Body Dysmorphic Disorder and Penile Enhancement: Understanding BDD, Small Penis Syndrome, and Treatment Limitations
AI automation is transforming the way businesses operate, from streamlining workflows to enhancing decision-making. In this article, we explore the latest trends, innovations, and real-world applications that are reshaping industries worldwide.
Introduction
Keywords: body dysmorphic disorder, penile enhancement, small penis syndrome, nonsurgical phalloplasty, penile fillers, male body image.
Body Dysmorphic Disorder (BDD) is increasingly relevant in modern aesthetic and sexual medicine, particularly in men seeking penile enhancement or nonsurgical phalloplasty.
Body Dysmorphic Disorder (BDD) is a psychiatric condition characterized by an excessive and persistent preoccupation with a perceived physical flaw that is either minor or entirely unnoticeable to others. This preoccupation causes significant distress, functional impairment, and often drives repetitive behaviors such as mirror checking, reassurance seeking, or avoidance of social situations.
While BDD can focus on virtually any body part, the genitalia—particularly the penis—represent a uniquely sensitive and emotionally charged focus. In aesthetic and sexual medicine, understanding BDD is essential, especially when evaluating men who present with concerns related to penile size, appearance, or proportionality.
Body Dysmorphic Disorder: A General Overview
BDD is classified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) under obsessive–compulsive and related disorders. Core features include:
Persistent preoccupation with a perceived physical defect
Significant distress or impairment in daily functioning
Repetitive behaviors (checking, comparing, camouflaging)
Poor insight or fixed beliefs about the defect
Importantly, reassurance from others—including medical professionals—rarely alleviates distress. In severe cases, patients may hold near-delusional convictions about their appearance.
BDD and the Penis: A Special Intersection
Concerns about penile size and appearance occupy a distinctive place in male body image. The penis is closely linked to identity, masculinity, and sexual confidence, making it a frequent focus for appearance-based anxiety.
Men with penile-focused BDD may:
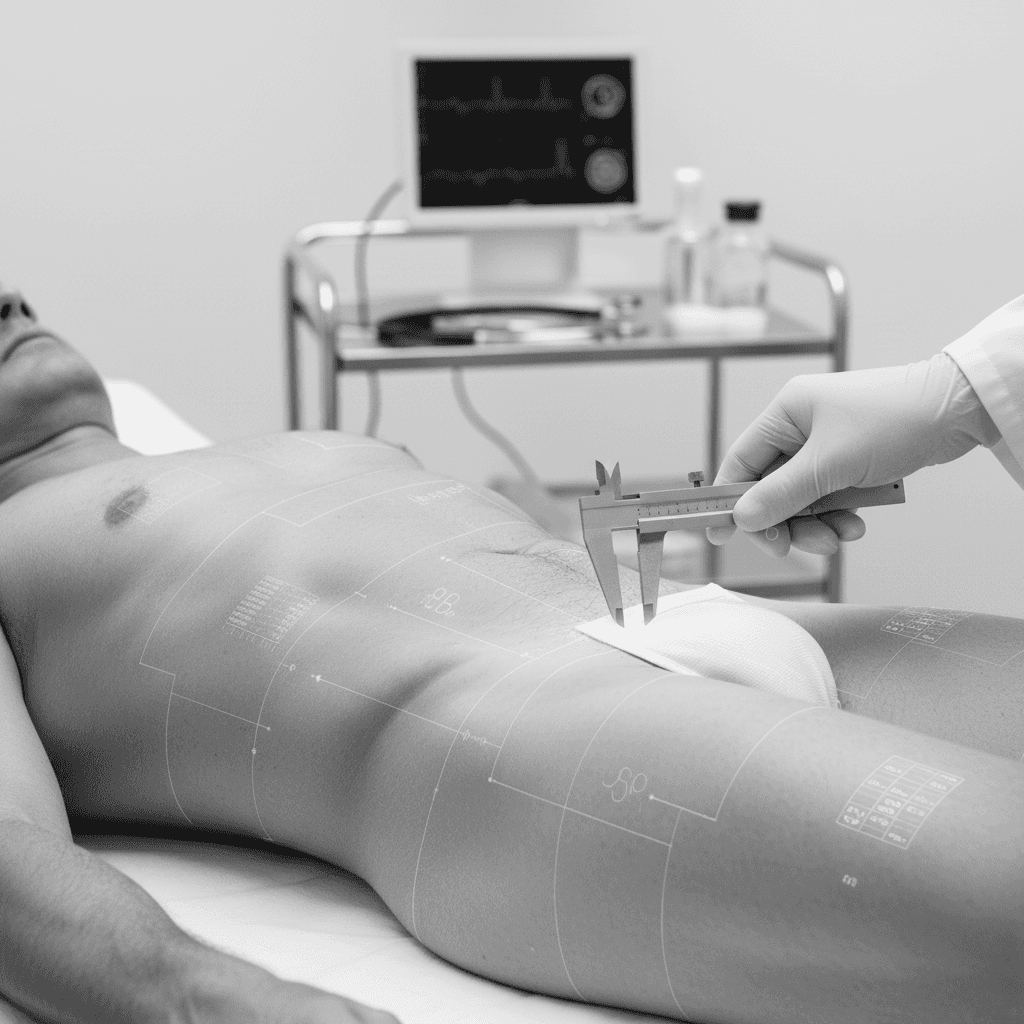
Spend excessive time measuring or comparing their penis
Avoid intimacy or sexual relationships
Experience intense shame or anxiety despite normal anatomy
Seek repeated medical or cosmetic consultations
Unlike general body dissatisfaction, penile-focused BDD is often hidden due to embarrassment, delaying proper diagnosis and treatment.
Small Penis Syndrome vs. Body Dysmorphic Disorder
Small Penis Syndrome (SPS) and BDD are related but not synonymous.
• SPS refers to distress over penile size in men whose measurements fall within normal statistical ranges. Many SPS patients are psychologically stable and capable of benefiting from reassurance or, in selected cases, physical intervention.
• BDD, by contrast, involves a deeper psychopathology in which perception is profoundly distorted and resistant to objective evidence.
• The clinical distinction is critical. While SPS exists on a spectrum of body image dissatisfaction, severe BDD represents a contraindication to cosmetic or enhancement procedures.
Why Severe BDD and Nonsurgical Phalloplasty Do Not Mix
Nonsurgical phalloplasty using soft-tissue fillers can produce real, measurable anatomical changes. However, in patients with severe BDD, objective improvement rarely translates into subjective satisfaction.
Key reasons include:
Unrealistic and Rigid Expectations.
Patients with BDD often hold fixed internal ideals that no realistic outcome can satisfy. Even technically excellent results may be perceived as inadequate or defective.
Perceptual Distortion Persists After Treatment.
BDD is not driven by anatomy but by altered perception. Enhancing the physical structure does not correct the underlying cognitive distortion.
High Risk of Dissatisfaction and Regret
Studies across aesthetic medicine consistently show higher rates of dissatisfaction, anger, and procedural regret among patients with untreated BDD.
Risk of Repetitive or Escalating Procedures
Patients may seek additional interventions in an attempt to resolve distress, increasing the risk of physical complications without psychological benefit.
For these reasons, responsible practitioners—including those at Avanti Derma—consider severe BDD a clear contraindication to nonsurgical penile enhancement.
Ethical and Clinical Responsibility
The ethical practice of aesthetic medicine requires more than technical skill; it demands discernment. Declining treatment for patients with severe BDD is not a rejection—it is an act of clinical responsibility.
Appropriate management includes:
Careful psychological screening
Honest discussion of limitations
Referral for mental health evaluation when indicated
When BDD is present, psychological treatment—not physical alteration—is the appropriate first-line therapy.
Screening Disclaimer
Important Patient Screening Notice:
Nonsurgical penile enhancement procedures are intended for psychologically stable patients with realistic expectations. Individuals with suspected or diagnosed Body Dysmorphic Disorder may experience persistent dissatisfaction despite technically successful outcomes. For this reason, patients exhibiting signs of severe BDD may be advised to pursue psychological evaluation and treatment prior to considering any form of penile enhancement.
Conclusion
Body Dysmorphic Disorder represents a profound disturbance of body perception, one that can significantly affect men concerned about penile size and appearance. While Small Penis Syndrome may respond to education, reassurance, or even carefully selected physical treatments, severe BDD does not.
In such cases, nonsurgical phalloplasty carries a high likelihood of dissatisfaction precisely because the problem does not reside in the anatomy. Recognizing this distinction protects patients from harm and preserves the integrity of aesthetic medicine.
True improvement begins when perception—not just proportion—is addressed.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing, 2013.
Veale, David. “Advances in a Cognitive Behavioural Model of Body Dysmorphic Disorder.” Body Image 12 (2015): 168–177.
Phillips, Katharine A. The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. Revised ed. Oxford: Oxford University Press, 2005.
Wylie, Kevan R., and David Eardley. “Penile Size and the ‘Small Penis Syndrome.’” BJU International 99, no. 6 (2007): 1449–1455.
Ghanem, H., et al. “Aesthetic Procedures and Psychological Outcomes in Male Genital Enhancement.” Journal of Sexual Medicine 15, no. 3 (2018): 277–286.
